The burnout epidemic in American medicine impacts over half of all doctors. More than ever before, physicians report feeling anxious, isolated and dissatisfied at work. Doctors have so soured on their profession, that 70% of them would not recommend a career in healthcare.
So what’s the problem? If you look closely at the self-reported surveys on burnout, it seems doctors already know exactly what’s wrong with their profession. Year after year, physicians identify the causes of their distress as “too many bureaucratic tasks,” “too many hours at work,” “increasing computerization,” and “insufficient compensation.”
All of these systemic issues in healthcare are, indeed, barriers to professional happiness. But if these surveys are correct, and doctors have correctly identified the healthcare system as the lone complication, why hasn’t the issue been solved? Perhaps it’s because doctors are simply helpless bystanders, unable to fix an already broken system. Or perhaps it’s because doctors have misdiagnosed a major part of the problem.
On Thursday, February 25, I had the opportunity to address this urgent topic at the Ending Physician Burnout Global Mini Summit. This online event was hosted by Jonathan Fisher, MD, FACC, a mindful and tireless advocate for the health of both doctors and their patients.
In my keynote address, I said that it is a mistake for doctors to decry the healthcare system as the sole cause of their burnout and moral grievances. When they do, they (1) imply that they’re powerless, (2) assume that they’re faultless, and (3) fail to see the problem from all sides.
Although it is true that physicians face an overly restrictive set of systemic requirements, doctors must also look in the mirror and acknowledge another major contributor to their distress: Their own culture.
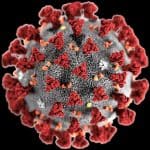
Physician culture is invisible yet highly influential. It shapes the thoughts, behaviors and actions of all doctors. It is inherited and expressed through rituals, customs, values and norms that get passed on from one generation of doctors to the next. It can be a virtuous force—leading to incredible scientific advancements whilst enabling doctors to provide exceptional care in some of the most dire circumstances, including the current Covid-19 pandemic.
But physician culture also carries a dark underbelly, a seedier side that often conflicts with the doctor’s vow to “first, do no harm.” Until doctors diagnose and treat this problem, their burnout crisis will continue.
As I told the 500-plus attendees at the Global Mini Summit, help won’t come to doctors until they address the elements of physician culture that contribute to healthcare’s high costs, low quality and the rising dissatisfaction of both patients and physicians.
To do so, doctors will need to work together to eliminate wasteful and ineffective medical care, including the 30% of tests and procedures that have been shown to add no value. Going forward, they must take responsibility for their failures in providing excellent preventive care (something the culture of medicine currently undervalues in relation to interventions). Physicians must do everything in their power to end unnecessary medical errors and reduce the complications of chronic disease. They must accept their role in the nation’s rising medical costs, stop suing patients who can’t afford to pay their out of pocket healthcare costs, stand up to the drug industry, and offer care that is both timely and convenient.
We all know the healthcare system is broken—well beyond the repairs that doctors, alone, can make. However, there are many opportunities to improve American medicine that are well within the reach and control of doctors.
Coming out of the coronavirus pandemic, physicians will have the opportunity to redefine “normal.” They can hold tight to the cultural norms and values of yesterday, and try to cling to the past. Or they can pursue a new normal. Those that step forward will be rewarded with a greater sense of purpose, fulfillment and satisfaction. In May, I will publish my next book, Uncaring: How the Culture of Medicine Kills Doctors & Patients, which offers physicians a new path forward—one that sets out to correct the failures of the U.S. healthcare system while also evolving the aspects of physician culture that harm patients and doctors alike.
* * *
Dr. Robert Pearl is the former CEO of The Permanente Medical Group, the nation’s largest physician group. He’s a Forbes contributor, bestselling author, Stanford University professor, and host of two healthcare podcasts. Pearl’s next book, “Uncaring: How the Culture of Medicine Kills Doctors & Patients,” is available for presale now. Follow him on Twitter @RobertPearlMD.




Dear Dr. Pearl,
Thank you for your insight and attention to this important topic. As a dedicated healthcare administrator, this is a very serious topic I try to monitor. It not only impacts clinical providers it impacts every staff member—the complexities in healthcare driven by IT demands and complex payer reimbursement models requires balance and focus.
Best regards,
Debra S. Mollohan, FACMPE