This month’s reader survey was inspired by a recent study on the power of primary care, which found that adding 10 primary care physicians to a population of 100,000 people is associated with an average life-expectancy increase of 51.5 days. That’s compared to a 19.2-day increase for an equal number of specialists. In other words, adding 10 primary care physicians has a 250% greater influence on life expectancy than an equivalent bump in specialists. The same survey determined that “the density of primary care physicians declined by 11% between 2005 and 2015, falling from 46.6 to 41.4 per 100,000 people.”
Unlike many other nations, the United States lacks a national strategy for making healthcare investments and right-sizing its healthcare workforce. Assuming we were to create such a strategy, please select which of these actions you would support:
1. Prevent hospitals from expanding in communities where there's already a surplus of hospital beds?
- Yes (65%, 41 Votes)
- No (29%, 18 Votes)
- No opinion (6%, 4 Votes)
Total Voters: 63
2. Limit new clinical services (cardiovascular, neurosurgical, etc.) when other hospitals in the same community have the capacity to accommodate patient needs?
- Yes (58%, 35 Votes)
- No (37%, 22 Votes)
- No opinion (5%, 3 Votes)
Total Voters: 60
3. Limit residency/fellowship positions for specialty training and divert those dollars to fund primary-care residencies?
- Yes (63%, 39 Votes)
- No (27%, 17 Votes)
- No opinion (10%, 6 Votes)
Total Voters: 62
4. Fund primary-care training opportunities for all "unmatched" medical school graduates?
- Yes (83%, 53 Votes)
- No (11%, 7 Votes)
- No opinion (6%, 4 Votes)
Total Voters: 64
All survey responses are anonymous. Cumulative results will be shared May 13, 2019 in the next issues of Monthly Musings On American Healthcare.
UPDATE: MARCH SURVEY RESULTS
I was surprised by the feedback in last month’s survey, specifically the optimism people had about the role technology will play in the future. There was near unanimous agreement that technology will untether physicians from their keyboards and allow patients to diagnose their own problems by the year 2030. Both of these developments would be positives.
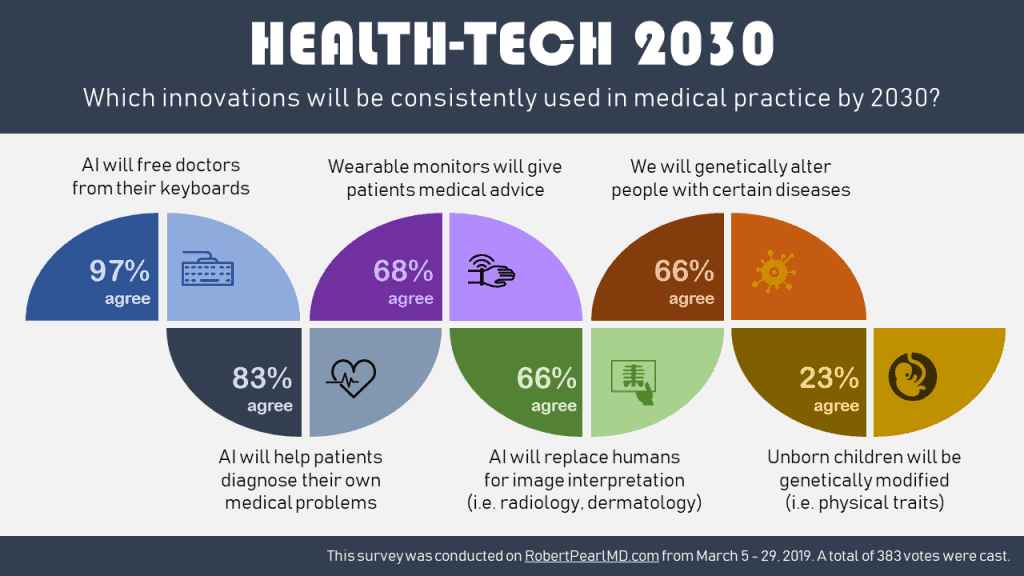
To facilitate the first innovation, we need to move away from fee-for-service billing, with its restrictive requirements around coding and documentation. For the latter, businesses will need the courage to translate medical knowledge into medical devices that help patients, despite the legal risks involved. So far, that hasn’t happened.
Similarly, when it comes to wearables and artificial intelligence, the limiting factor isn’t the technology. It’s society’s unwillingness to forgive mistakes that come from machines. We accept that “to err is human,” but we expect technology to be perfect. Even a recommendation, interpretation or conclusion that is 99.99% accurate will be wrong once every 10,000 times. And when it happens, it makes page news and goes viral on social media.
Survey respondents were less confident about the impact of genomics in the future. The technology for genetic alteration has made huge leaps forward. But as recent coverage from China shows, the application of CRISPR on humans remains controversial.
* * *
Dr. Robert Pearl is the former CEO of The Permanente Medical Group, the nation’s largest physician group. He’s the bestselling author of “Mistreated: Why We Think We’re Getting Good Health Care–And Why We’re Usually Wrong” and a Stanford University professor. Follow him on Twitter @RobertPearlMD.



IMHO the problem is artificial restraints on medicine. I am one of those libertarian leaning people who think getting rid of government intervention is the easy way to solve many of our nation’s problems. Let the free market decide what money flows wherever. Now I know this is currently hopeless to achieve on a national level, so let me propose a reasonable solution. Take a very small part of the USA (let’s say an under served county of West Virginia) and divide it in half for medical services. One half will become a medical free enterprise zone in which all government medical intervention is jettisoned. The other half becomes whatever the current best liberal thinking in the USA considers to be optimal. See what happens. Medical care will become much less expensive in the free enterprise zone. It might even become better – and I am sure many who read this will disagree. But wouldn’t it be nice to know for sure?
It is hard to fill out such a survey. The example of primary care stands out.
There is nothing that can be done in GME, special GME, or MD DO NP PA training to fix deficits. These are entirely about the financial design paying the least where shortages exist and penalizing practices most with additional costs of delivery. Proper treatment requires a proper assessment – not assumptions that more graduates or special training will work.
There are simply too few dollars to support US primary care and even less for primary care where needed across 75% of the rural population, 32% of the urban population, and 40% of the nation overall with just 25% of generalists and general specialists.
The worst public and private plans are concentrated in these counties. They did not lack insurance greater than other US populations, they just had the worst that treat patients and providers the worst. Small, basic, cognitive, office, most needed, less organized, poor awareness, and away from concentrations are what work against their needs.
They are also growing fastest in numbers, demand, and complexity while their workforce is held flat, their hospitals are closed, and their providers are penalized because they remain and care for patients with inherently lower outcomes (situations, conditions, environments, and other associations with poor health).
These practices have the highest levels of disruptions to address including highest turnover. Fix the financial design to fix primary care, mental health, general surgery, women’s health, and care where needed.
A very different framework is needed. Not expansion of insurance, but revenue greater than the costs of deliver. Not regulation, innovation, and digitalization, but support of the team members who deliver the care. And certainly not cost cutting and overutilization focus where numerous barriers to care have existed for decades and will continue to exist until the financial design is changed.
The first question should always be what do the patients need in any community. Not the system, not the business, not the political party but each individual patient. Always need a patient centered umbrella (context) for every question.