More than half of the country’s 525 Medicare ACOs count themselves as members of the National Association of Accountable Care Organizations (NAACOS), where I had the pleasure of speaking on Oct. 5. The participating organizations are at the cutting edge of healthcare change. And although they vary in geography, size and structure, they all understand the current healthcare system is broken and that innovative transformation is key to fixing it.
Done well, ACOs can enhance quality of medical outcomes, improve patient convenience and reduce cost. They bring together physicians, hospitals and health plans in redesigning how medical care is structured, reimbursed and technologically supported. They serve tens of millions of patients and represent the future of American healthcare. And that’s why the NAACOS Fall 2017 meeting was aimed at helping ACOs achieve their goals by delivering valuable policy insights and operational strategies.
The association’s mission is to foster growth of the ACO model, help all groups improve quality and reduce costs, and participate with federal agencies and elected officials in developing and implementing effective public policy. NAACOS is led by Clif Gaus, a visionary leader who not only understands the potential of the model, but is committed to creating the research methodologies required to understand how they can best provide superior quality, make coverage affordable, and help ensure convenient and rapid patient access and to care.
This year’s program began with a keynote from Mark McClellen, the former administrator of the Centers for Medicare and Medicaid Services (CMS) and previous Commissioner for the Food and Drug Administration (FDA). For three days, the program included both didactic sessions and shared-learning experiences. More than 600 attendees found the program powerful, inspiring and educational.

My talk focused on the challenges of healthcare today, and the crucial role ACOs will play in the future. I emphasized the difficulties ACOs have in making the transition from the traditional model of the past –markedly fragmented, technologically limited, fee-for-service based and without a strong leadership – to one appropriate for the 21st century. I highlighted the superior quality, added convenience and lower costs that can be achieved when care is (a) integrated both within and across specialties, (b) paid through a capitated approach that rewards outcomes rather than volume, and (c) reliant on modern technology, including both video/mobile communications with patients and a comprehensive electronic health record (EHR) that contains the totality of a patient’s information.
I then acknowledged and offered my thoughts on the challenges of moving to this new model. Given the eclectic nature of the over 200 organizations in the room, I pointed out three huge hurdles that need to be overcome:
- Right-sizing the ACO. When a hospital system and physician leaders come together to design a next-generation approach to healthcare, they quickly realize they need fewer doctors, particularly specialists, and fewer hospitals. Higher patient volumes for physicians and facilities help improve quality outcomes and allow economies of scale. But as soon as the new ACO announces who is included and who is not, those excluded are likely to take their patients elsewhere, and the economic loss can bankrupt the hospital. As such, everyone tends to be included, and therefore improvements in performance and cost reduction are slow.
- Fee-for-service payments. When the ACO is forming, the participating doctors frequently participate not only in the ACO, but also in a variety of other insurance programs. As Shannon Brownlee says, “It is like having one foot in each of two canoes.” It is difficult for them to provide the higher value care of the ACO, and as a result, they are slow to improve preventive care and utilization. Leaders of the ACO know that if all doctors were on an annual salary and offered incentives for higher quality and patient service, care would improve. Getting there, especially early on, is the hard part.
- The shortage of physician leadership. Doctors in medical school are not trained in the skills required to be effective leaders. Leadership is similar to making complex diagnoses or performing surgery: It requires training and experience. For ACOs, developing physician leaders throughout the organization is essential, but the cost of training often is prohibitive. In this way, it is similar to a capital investment with a high up-front expense that requires many years to recoup ROI. As such, that step is usually underfunded during the embryonic period for a new ACO.
My hope is that our nation will recognize the groups in the room at the NAACOS Fall Conference represent the right solutions to the shortcomings of American healthcare today. Possibly, the new payment mechanisms built in through MACRA will provide some of the dollars needed to help these organizations make the transition. Maybe innovative partnerships between these ACOs, health plans and businesses will allow the short-term changes needed for long-term growth and success. I will continue to encourage these types of relationships and care delivery improvements.
Those of us who have led in organizations like Kaiser Permanente, Mayo Clinic or Geisinger have the massive advantage of having inherited medical groups and hospital systems with decades of history and progressive growth over time. For the newer programs, the hill is steep. But once they get to the top, the value created for their patients will be immense.
I left the NAACOS Fall Conference optimistic that the association will find new and innovative ways to address the healthcare challenges our nation faces. I encourage others to join the bandwagon and, together, make our nation’s healthcare the best in the world.
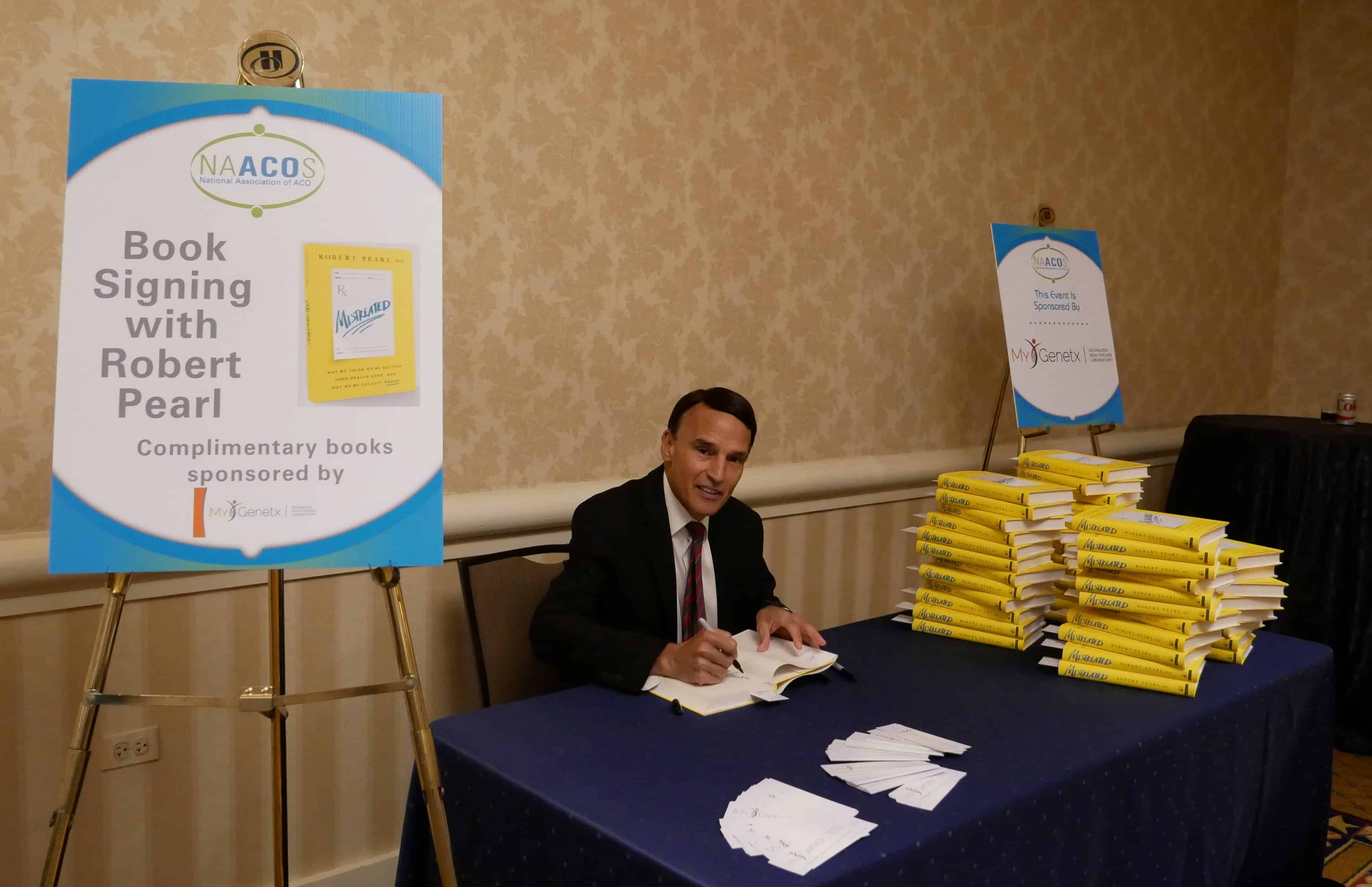
Dr. Robert Pearl is the bestselling author of “Mistreated: Why We Think We’re Getting Good Health Care–And Why We’re Usually Wrong” and a Stanford University professor. Follow him on Twitter @RobertPearlMD.