This event was an opportunity to discuss artificial intelligence in healthcare and also a chance to challenge traditional thinking about how we define and measure the quality of U.S. healthcare.
 A shift in focus: From processes to outcomes
A shift in focus: From processes to outcomes
During our conversation, we discussed the limitations of our nation’s stubborn focus on “healthcare processes” rather than on what truly matters: outcomes.
In today’s world, we measure success by evaluating specific actions—how many screenings are done, how often blood pressure is taken or whether flu shots are administered on time. These are important tasks and they matter. But they aren’t the ultimate goal. What we want is better patient health and fewer complications at more affordable costs.
Peggy and I took time to envision a healthcare system driven not by checkboxes but by clinical results.
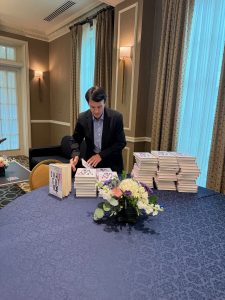
This shift in thinking is critical as we look to leverage the power of generative AI. As I detailed in my book, ChatGPT, MD (for which all profits go to Doctors Without Borders), the transformative potential of GenAI isn’t in its ability to automate processes. The technology’s power lies in its ability to improve patient outcomes and reduce clinician burden. AI can speed up tasks. But, more importantly, it can enhance medical quality by focusing on holistic and measurable improvements in the health of patients.
The role of AI in bridging the gap
 AI applications are already being used to interpret mammograms and diagnose conditions like pneumonia with high accuracy and consistency. But the technology’s greater potential extends far beyond radiology.
AI applications are already being used to interpret mammograms and diagnose conditions like pneumonia with high accuracy and consistency. But the technology’s greater potential extends far beyond radiology.
Chronic diseases like diabetes, hypertension and heart failure place increasing demands on clinicians and compromise outcomes. Currently, healthcare providers control hypertension in only 60% of patients, while diabetes is effectively managed even less often. By using generative AI tools connected to home monitoring systems and wearable devices, patients and doctors can be alerted when medications are not adequately controlling these conditions. This allows for faster, more precise adjustments to treatment plans, often without the need for in-person visits.
Advancing quality with GenAI and equity in mind
One of the key themes at this year’s summit was the emphasis on equity. At NCQA, the mantra is clear: “There can be no quality without equity.”
AI can help close the gaps in healthcare access and outcomes, but only if it’s implemented responsibly and equitably. A major concern in this digital age is the growing divide between those who have access to health technology and those who do not. AI, if properly integrated, has the potential to level the playing field.
In my Forbes piece earlier this year, I introduced the concept of “GenAI-Driven Health Hubs”—community-based centers that could bridge the digital divide by offering access to AI-based healthcare solutions for people with chronic conditions in underserved areas. I believe that by piloting AI initiatives in these hubs, we can expand its positive impact for vulnerable populations and narrow the gap in health outcomes based on socioeconomic factors.
Redefining healthcare payments and quality measures
During the chat, Peggy and I explored the importance of embracing new healthcare reimbursement models in healthcare. For AI to reach its full promise in medicine, we need to fundamentally change how we pay for medical care.
The current fee-for-service (FFS) system incentivizes providers to deliver more services rather than to improve health outcomes. In this transactional model, clinicians are rewarded for performing more procedures and seeing more patients, which results in rushed appointments, fragmented care and physician burnout.
The solution lies in shifting from FFS to a value-based model, such as capitation. Under capitation, doctors and hospitals receive a fixed annual fee to manage the health needs of a defined patient population, rewarding quality outcomes over service volume. This model encourages providers to focus on preventive care, chronic disease management and teamwork, which can ultimately reduce costs and improve health outcomes.
The CDC estimates that better management of chronic diseases could reduce the rates of heart attacks, strokes, cancers and kidney failures by 30-50%. In a fee-for-service system, such reductions would be financially disastrous, greatly diminishing doctor and hospital revenue. But in a capitated model, these same improvements benefit both patients and providers.
As I explored in ChatGPT, MD, AI can support this shift toward a value-based mindset by identifying at-risk patients, monitoring treatment adherence and offering real-time, personalized interventions. For example, in diabetes care, generative AI can monitor blood glucose, provide medication reminders and suggest treatment adjustments based on blood glucose trends over time.
Transitioning to capitation, however, will require bold leadership, innovative thinking and effective communication, as well as specialized training for doctors in collaborative and cooperative care practices.
As I depart Nashville, I want to thank Peggy O’Kane and the NCQA team for hosting this year’s Health Innovation Summit. Their dedication to advancing healthcare quality inspires us to work together in making American healthcare the best in the world once again.
For those interested in exploring these ideas further, I encourage you to read ChatGPT, MD, where I dive deeper into AI’s potential to transform American medicine.
* * *
Dr. Robert Pearl is the former CEO of The Permanente Medical Group, the nation’s largest physician group. He’s a Forbes contributor, bestselling author, Stanford University professor and host of two healthcare podcasts. Check out Pearl’s newest book, ChatGPT, MD: How AI-Empowered Patients & Doctors Can Take Back Control of American Medicine with all profits going to Doctors Without Borders.